Mucopolysaccharide (MPS)
As an organization, we have managed to identify individuals with Mucopolysaccharide (MPS) disease.
Mucopolysaccharide (MPS) diseases are a family of rare, life-limiting lysosomal storage disorders that can affect both children and adults. According to MPS Society UK, Mucopolysaccharides are long chains of sugar molecules used in the building of bones, cartilage, skin, tendons, and many other tissues in the body. Usually, there is a continuous recycling process of building new mucopolysaccharides and breaking down old ones. For people with MPS diseases, there is not enough of a particular enzyme to break down used mucopolysaccharides which means they build up and store in the cells in the body which causes progressive damage.
Who are at Risk?
Estimates indicate that approximately one in every 25,000 babies born will have some form of mucopolysaccharidoses. These are autosomal recessive disorders, meaning that only individuals inheriting the defective gene from both parents are affected. When both parents have one copy of the defective gene, each pregnancy carries with it a one in four chance that the child will be affected. The parents and siblings of an affected child may have no sign of the disorder. Unaffected siblings and select relatives of a child with one of the mucopolysaccharidoses may carry one copy of the defective gene and could pass it on to their own children.
In general, the following factors may increase the chance of having or passing on a genetic disease:
- A family history of a genetic disease
- Parents who are closely related or part of a distinct ethnic or geographically clustered community
- Parents who do not show disease symptoms but carry a disease gene.
Family Screening
MPS I is an inherited disorder, family screening is extremely important. When a diagnosis for an individual is made, it is important to find out whether other siblings may also be affected. A genetic counselor can be a valuable resource to help you understand how MPS I is inherited in families, and to help determine if others in the family would want to consider genetic testing for MPS I as well.

Did you know?
May 15th is International MPS Awareness Day. Join us every year as we support raising awareness of MPS disease disorders and honoring the individuals and families who are affected.
What are the signs and symptoms?
The mucopolysaccharidoses share many clinical features but have varying degrees of severity. These features can or may not be apparent at birth but progress as the storage of glycosaminoglycans affects bone, skeletal structure, connective tissues, and organs. The age of presentation varies widely.
Stiffened Joints
Stiffness of joints may cause pain and limited range of movement and may create challenges with dressing and other activities.
Skeletal Problems
Skeletal problems can include problems with growth and bone formation, including abnormally shaped bones. The spine can also be affected, including spinal deformities such as scoliosis and poorly formed spine.
Carpal Tunnel Syndrome
A condition that causes pain, numbness, and tingling in the hand and arm. This may cause nerve damage and challenges grasping objects.
Heart Disease
Some types of heart problems that occur in people living with Hurler include: weakened heart muscle, stiffened and scarred heart, and coronary artery disease. Patients living with MPS I disease also may develop problems with their heart valves.
Upper Airway Infections
Upper airway infections include bacterial infections that occur in the middle area of the ear and sinuses.
Obstructive Sleep Apnea
Obstructive sleep apnea is a potentially serious sleep disorder that causes the muscles in the throat to relax and block the airway during sleep, which causes breathing to repeatedly stop and start.
Corneal Clouding
The cornea can become cloudy, which can limit vision.
Spinal Cord Compression
Spinal cord compression occurs when fluid or tissues press against the spinal cord, which can cause numbness, pain, and weakness.
Enlarged Liver and Spleen
Hernia
In people with MPS I, a hernia which is a bulge in the abdomen or groin, can occur. Hernia can often be harmless and pain-free, but at times it can bring discomfort and pain.
Hearing Loss
Delayed Cognitive Development
Coarse Facial Features
People living with MPS I can have large heads, flat faces, shallow eye sockets, large tongue, and broad, short noses.
Fluid on the Brain (Communicating Hydrocephalus)
A condition in which the clear fluid that surrounds the brain and spinal cord builds up and causes pressure on the brain.
Abnormally Shaped Teeth
The outer layer of the teeth, known as the enamel, can be fragile and there can be poor teeth formation.
Life expectancy
Life expectancy varies significantly for people with MPS I. This depends on many factors, such as where they are on the spectrum of disease severity, and management of its signs and symptoms. People with MPS also have a significantly shortened life span. Some individuals who are more severely affected may die before becoming teenagers, while others may live to be adults. The most severely affected children (those with what was historically known as Hurler Syndrome) rarely live more than 10 years.
MPS In Zimbabwe
There are no known statistics to verify the number of people in Zimbabwe with MPS. As an organization, we have managed to identify two individuals with MPS. However, it is unfortunate to note that the most recent individual identified passed away in 2021 due to pneumonia. We currently offer psychosocial support and medicine for our one MPS patient and are in the process of identifying and tracing more people with MPS ( if any ).
Supportive and symptom-based management
Since MPS I is a multi-systemic disease, the care of an MPS I patient can involve many specialists. Patients with MPS I may require supplemental oxygen, continuous positive airway pressure, or tracheostomy for breathing difficulties. Surgery may be necessary for spinal cord compression, hernia repair, carpal tunnel syndrome, or heart valve replacement. Physical therapy can help with joint stiffness.
Hemophilia and Von Willebrand Disease (VWD)
As an organization, we have managed to identify a number of individuals who have different rare conditions and are currently in the process of setting up different groups for them, one of the rare conditions we have identified is Hemophilia.
In people with bleeding disorders, the clotting process doesn’t work properly. As a result, people with bleeding disorders can bleed for longer than normal, and some may experience spontaneous bleeding into joints, muscles, or other parts of their bodies.
Hemophilia is a bleeding disorder that affects approximately 1 in 10,000 people. People with hemophilia do not have enough clotting factor VIII or IX in their blood. As a result, they can bleed for longer than normal. The most common bleeding disorder is von Willebrand disease (VWD). It is generally less severe than other bleeding disorders. Many people with VWD may not know that they have the disorder because their bleeding symptoms are very mild. Clotting factors are proteins in the blood that control bleeding. When a blood vessel is injured, the walls of the blood vessel contract to limit the flow of blood to the damaged area. Then, small blood cells called platelets stick to the site of injury and spread along the surface of the blood vessel to stop the bleeding.
Hemophilia has different levels of severity ranging from mild, moderate, and severe. Mild (6%-49% factor level) – problems with bleeding only after serious injury, trauma, or surgery. The first episode may not occur until adulthood and is not discovered until a major injury or surgery or tooth extraction. Moderate (1%-5% factor level) – bleeding episodes after injuries and also after major trauma or surgery. Occasional bleeding episodes without obvious cause take place and these are called spontaneous bleeding episodes. Severe (less than 1% factor level) – bleeding following an injury or surgery and may also experience spontaneous bleeding into joints and muscles. The severity of hemophilia doesn’t change over time in a given individual. However, there is one exception which is a special form of hemophilia B called hemophilia B Leiden.
The most common symptom is bleeding especially into joints and muscles, symptoms of these bleeds include pain, swelling, inability to move or use the affected body part. Young infants may bleed in their mouths whereas toddlers and older children commonly bleed into muscles and joints. Another symptom is prolonged nose bleeding, vomiting of blood, and easy bruising. A person with hemophilia bleeds longer than a person without hemophilia. Heavy menstrual bleeding, which may lead to low iron levels or anemia.
Hemophilia In Zimbabwe
In Sub-Saharan Africa, Hemophilia remains a huge problem mainly because of ignorance of the disease, limited screening capabilities, and access to treatment.
In Zimbabwe, research has shown that there is no national data on Hemophilia, but it is estimated that about 500 people are living with Hemophilia. Currently, there are only 2 hospitals that have Hemophilia Clinics in Zimbabwe which are Parirenyatwa in Harare and Mpilo in Bulawayo. The shortage in Hemophilia clinics has thus posed a threat to the Hemophiliac community as there is limited access to health care services. Presently, in Zimbabwe tests for Hemophilia cost at least US$200 and are carried out in South Africa as there are no equipped laboratories locally to carry out the procedure.
Treatment
Although there is no cure for hemophilia, effective therapies have been developed. Most affected individuals can lead full, productive lives by maintaining proper treatment and care. Acute bleeding episodes are treated with clotting factors, which should be administered immediately to prevent hemarthroses, compartment syndrome, or ICH. Prophylactic replacement therapy should be implemented for individuals with severe bleeding. This treatment reduces episodes of bleeding and also prevents the development of arthropathy and compartment syndrome. Hormone treatment such as oral contraceptives (birth control pills) can help women who have heavy menstrual bleeding. The hormones can increase factor VII levels.
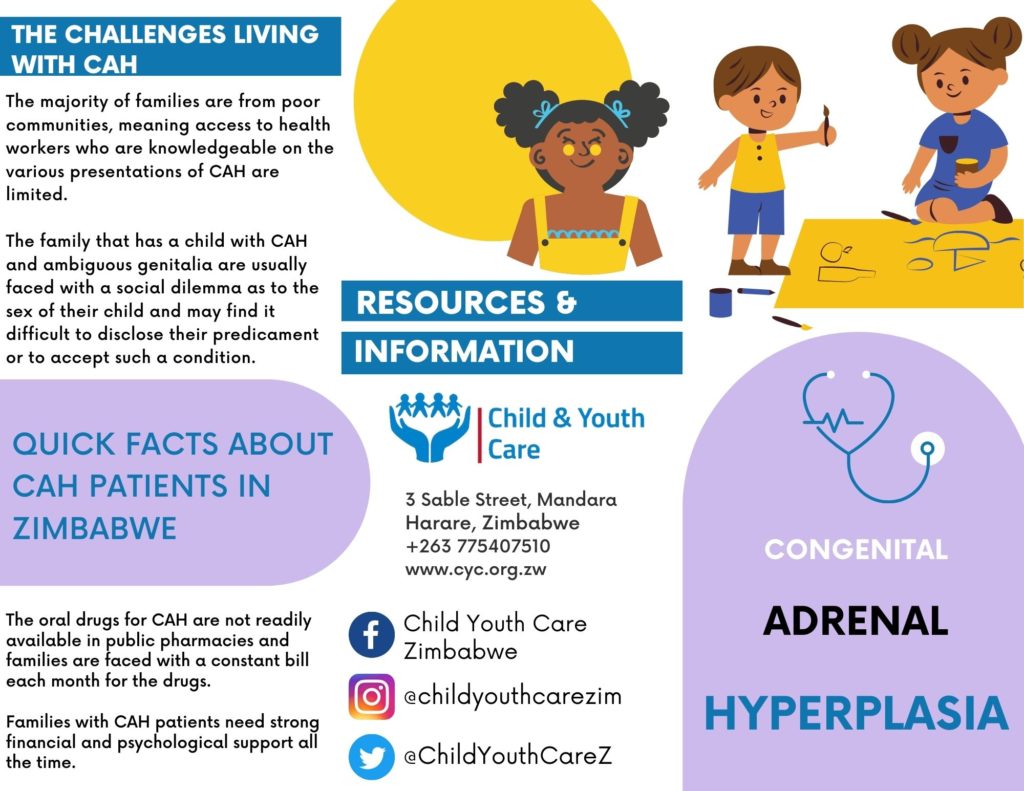
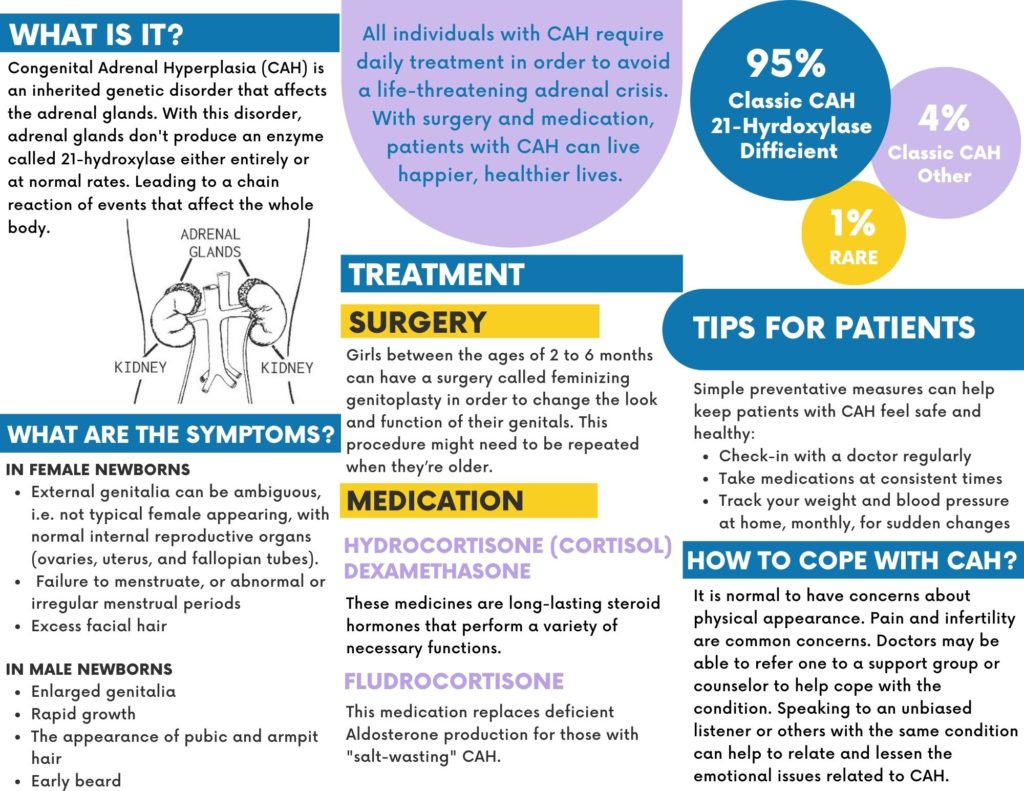
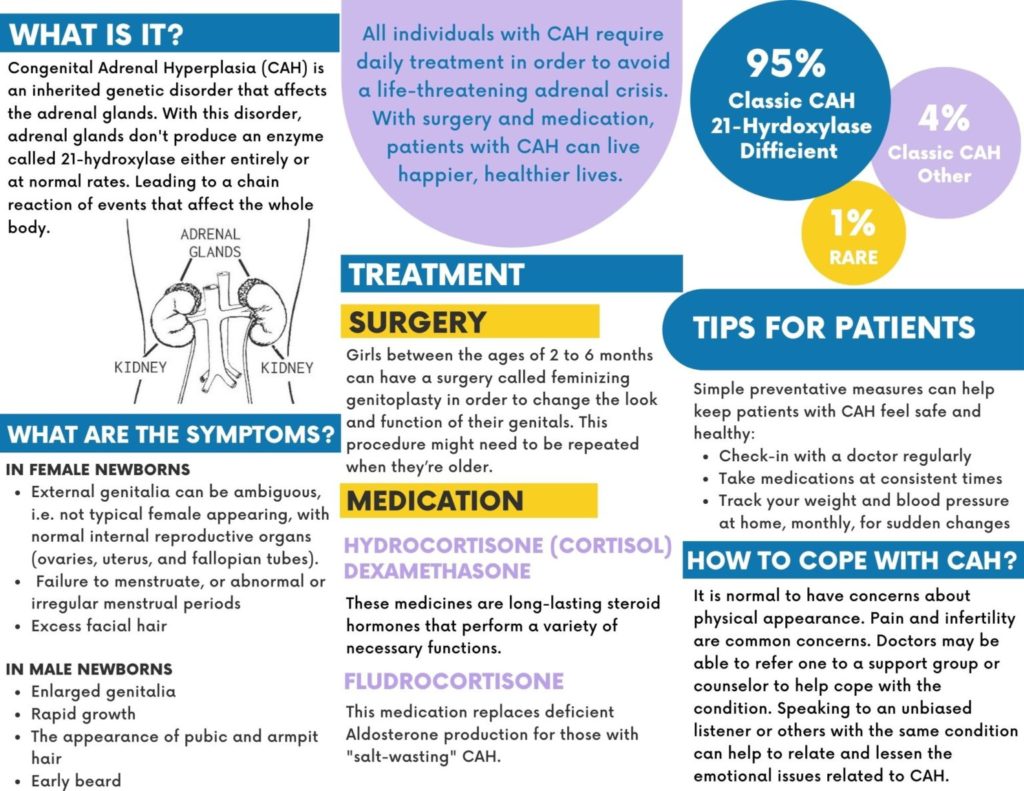
Congenital Adrenal Hyperplasia (CAH) Beneficiaries
At Child and Youth Care (CYC), we aim to empower vulnerable and neglected children who are affected by Congenital Adrenal Hyperplasia (CAH). Our mission is to defend, champion, and advance the interests of children living with CAH and their caregivers so as to improve their quality of life. We aim to provide the much-needed intervention in supporting children living with (CAH) by setting up different support groups and by making an early diagnosis, treatment and care more accessible through the help of local and international stakeholders.
Background and Problem
Congenital adrenal hyperplasia is a group of rare genetic conditions that limit the production of essential hormones in the adrenal gland. The adrenal gland is a small organ above the kidneys that produce hormones such as cortisol, aldosterone, and androgens. Individuals who have CAH lack certain enzymes needed to make such hormones as cortisol and aldosterone. This condition does not have a cure. It can be detected at birth, during early childhood, or early adulthood. It is a life-threatening condition but with proper treatment affected individuals can lead normal lives. Affected individuals could present with ambiguous genitalia, meaning their external sexual organs are neither clearly male nor female, can present with adrenal crisis, a life-threatening situation, short stature, early puberty, early pubic hair appearance, or irregular periods. Treatment includes lifelong hormonal medications, surgery to correct the external sexual anatomy, and counseling for the individual and family.
CAH in Zimbabwe
In Zimbabwe, children with CAH face a myriad of challenges.
- Diagnosis requires a health worker who is knowledgeable on the various presentations of CAH and who knows how urgent it would be to refer that child timeously as well as where to refer.
- The family that has a child with CAH and ambiguous genitalia are usually faced with a social dilemma as to the sex of their child and may find it difficult to disclose their predicament or to accept such a condition
- Children with an adrenal crisis are at high risk of death if appropriate treatment is not instituted urgently. This requires a health center that has knowledgeable health workers and correct medications to treat this emergency
- Having survived these crises, families need to be empowered on avoiding such medical emergencies and having their own drug stocks in case this happens again.
- Individuals with CAH have usually prescribed cortisol plus or minus fludrocortisone as lifelong therapy. These oral drugs are not available readily in public pharmacies and families are faced with a constant bill each month for such drugs.
- Surgical intervention is usually required for females with CAH and this is usually only offered in quarterly health facilities. Psychological support for such families is key.
The overarching goal is to assist in the mobilization and create awareness of children living with CAH so that they can demand their social, political, economic, and physical rights from various duty bearers. We also aim to capacitate the families for early diagnoses, care, and social inclusion.
Our organization works within the framework of global health coverage for all, this creates a need to lobby and advocate for policies and laws that are sensitive to the needs of children living with CAH. Ultimately, CYC seeks to support the government in developing CAH friendly policies and to ensure that medical support is extended to CAH patients as well as provide humanitarian support to the patients and their families. Our theory of change is anchored on improving the quality of life of people living with CAH. Our long-term vision is to develop a detailed and database that can be used nationally and regionally but most importantly to realize improved living conditions.
Classic Galactosemia (CG)
Through our, We Love Rare initiative program and referral doctors we managed to identify children with a new rare disease called Classic Galactosemia (CG)
Galactosemia is a rare, hereditary disorder of carbohydrate metabolism that affects the body’s ability to convert galactose to glucose. Galactose is a sugar contained in milk, including human mother’s milk as well as other dairy products. It is also produced by the human body, and this is called endogenous galactose. This means that even if children with CG do not consume milk they are still at high risk of falling ill as the body thinks galactose is toxic or poisonous. Research has shown that children who follow a lactose-restricted (dairy-free) diet is absolutely essential to avoid profound intellectual disability, liver failure, and death in the newborn period. Classic galactosemia can result in life-threatening health problems unless lactose is removed from the diet shortly after birth.

Signs & Symptoms
An infant with galactosemia appears normal at birth, but within a few days or weeks loses their appetite and starts vomiting excessively. Yellowing of the skin, mucous membranes, and whites of the eyes (jaundice), enlargement of the liver (hepatomegaly), the appearance of amino acids and protein in the urine, growth failure, and, ultimately, accumulation of fluid in the abdominal cavity (ascites) with abdominal swelling (edema) may also occur. Diarrhea, irritability, lethargy, and a bacterial infection may also be early signs of galactosemia. In time, wasting of body tissues marked weakness, and extreme weight loss occur unless lactose is removed from the diet. Long-term complications also show in a minority of these children, developmental delay and/or a speech abnormality occurred, but it is unclear whether this is related to an accumulation of galactose and its metabolites.
Affected Populations
Classic galactosemia is diagnosed in the range of 1/16,000 to 1/48,000 births through newborn screening programs around the world, depending on the diagnostic criteria used by the program. The disorder has been reported in all ethnic groups. An increased frequency of galactosemia occurs in individuals of Irish ancestry.
Standard Therapies
Treatment
Infants and children with galactosemia should have a lactose-restricted (dairy-free) diet that contains lactose-free milk substitutes and other foods such as soybean products. Fortunately, infants with galactosemia can synthesize galactolipids and other essential galactose-containing compounds without the presence of galactose in food. Therefore, satisfactory physical development is largely possible if a strict diet is followed. The emotional effects of the strict diet may require attention and supportive measures throughout childhood.
Speech therapy may be necessary for children with childhood apraxia of speech or dysarthria. For school-age children, individual education plans and/or professional help with learning skills may be necessary for some individuals, depending on psychological developmental assessments.
Unfortunately, it has been found that there is no treatable cure for children living with CG. Awareness needs to be focused on finding a reliable treatment for galactosemia.